Acute Liver Failure: A Comprehensive Overview on Diagnosis, Management, Prevention & Herbal Remedies
Table of Contents
ToggleIntroduction
Acute Liver Failure (ALF) is a rare but life-threatening condition that demands immediate medical attention. This comprehensive guide delves into the various aspects of ALF, including practice essentials, clinical presentation, differential diagnosis, workup, conventional treatment, prevention, herbal medicines, lifestyle modifications, and concludes with vital insights for those affected by this challenging condition.
Practice Essentials of Acute Liver Failure
Understanding the fundamental aspects of Acute Liver Failure is essential for healthcare professionals and patients alike. Let’s explore the practice essentials of this critical condition.
- Definition and Incidence
Acute Liver Failure is characterized by the rapid onset of severe liver dysfunction. Unlike chronic liver disease, which develops gradually, ALF occurs suddenly and is often a life-threatening emergency. It is relatively rare, with an annual incidence of approximately 1-6 cases per million individuals.
- Etiology
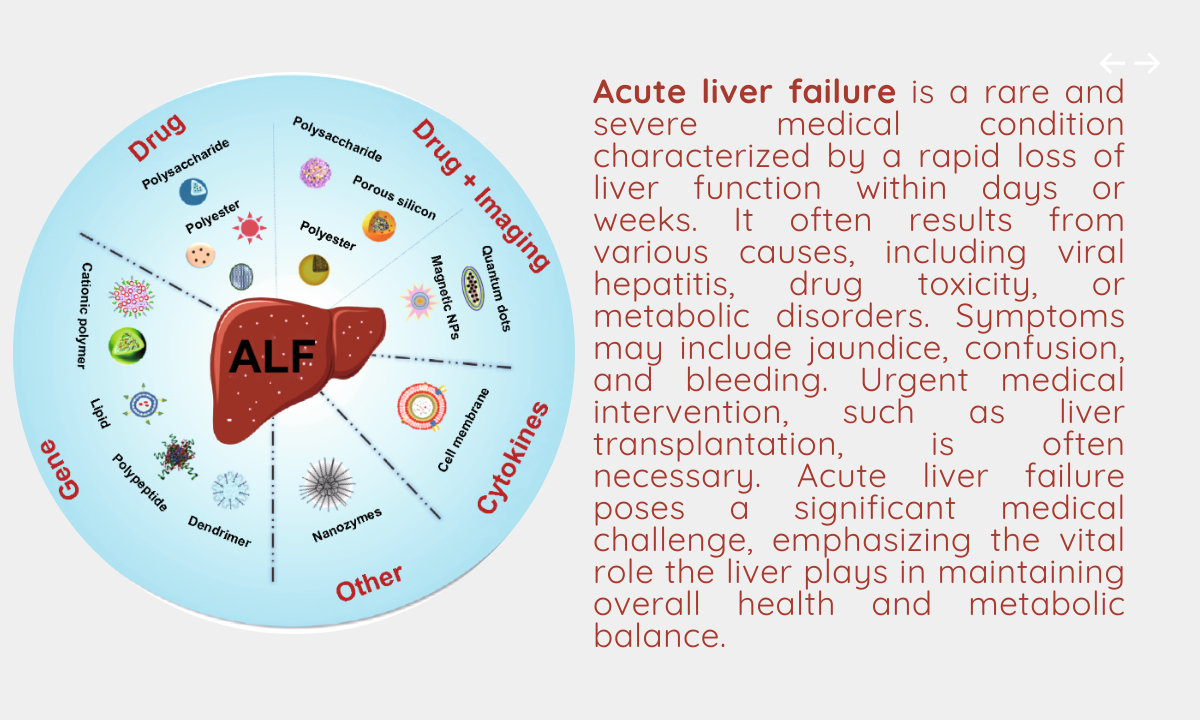
ALF can be caused by various factors, including viral hepatitis, drug-induced liver injury, autoimmune conditions, and metabolic disorders. Identifying the underlying cause is crucial for effective management.
- Clinical Progression
The condition progresses rapidly, often leading to hepatic encephalopathy, a severe impairment of brain function due to the liver’s inability to clear toxins from the blood. This can result in confusion, coma, and, in severe cases, cerebral edema, which is a life-threatening complication.
Clinical Presentation of Acute Liver Failure
ALF presents with a range of symptoms and signs that reflect the liver’s inability to function properly. The clinical presentation may include:
- Jaundice
Jaundice, characterized by yellowing of the skin and eyes, is a common symptom. It occurs due to the accumulation of bilirubin in the bloodstream.
- Hepatic Encephalopathy
Cognitive impairment and changes in mental status are hallmark features of ALF. This can range from confusion and disorientation to severe coma.
- Gastrointestinal Symptoms
Patients may experience nausea, vomiting, and abdominal pain.
- Coagulopathy
The liver plays a critical role in blood clotting, and its dysfunction can lead to easy bleeding and bruising.
- Fatigue and Weakness
Patients often report profound fatigue and weakness.
- Ascites and Edema
Accumulation of fluid in the abdomen (ascites) and swelling of the legs (edema) can occur.
It’s important to note that ALF can progress rapidly, leading to life-threatening complications. Therefore, immediate medical attention is crucial.
Differential Diagnosis
ALF shares some clinical features with other medical conditions, and it’s essential to consider these in the differential diagnosis. Conditions that may mimic ALF include:
- Chronic Liver Disease
While ALF is characterized by sudden liver dysfunction, chronic liver diseases, such as cirrhosis, develop over an extended period. It’s crucial to differentiate between these conditions.
- Hepatitis A, B, or C
Acute viral hepatitis can present with jaundice and liver dysfunction, but ALF progresses more rapidly and severely.
- Drug-Induced Liver Injury
Medications or toxins can lead to liver injury and may present with symptoms similar to ALF. Distinguishing between the two is crucial for treatment.
- Wilson’s Disease
This genetic disorder can cause copper accumulation in the liver and brain. Symptoms can mimic ALF, making it important to consider Wilson’s disease in the differential diagnosis.
- Hemolysis
Excessive breakdown of red blood cells (hemolysis) can result in elevated bilirubin levels and jaundice, resembling ALF.
A comprehensive medical evaluation, including history, clinical examination, and laboratory tests, is essential to distinguish ALF from these conditions.
Workup for Acute Liver Failure
The workup for ALF involves a series of diagnostic tests and procedures to identify the underlying cause and assess the severity of liver dysfunction:
- Medical History and Physical Examination
A detailed medical history and thorough physical examination are conducted to identify potential risk factors, symptoms, and signs of ALF.
- Laboratory Tests
- Liver Function Tests: These tests evaluate the liver’s synthetic and detoxifying functions. Elevated levels of liver enzymes (AST and ALT) and bilirubin are common in ALF.
- Coagulation Profile: Assessment of blood clotting parameters helps evaluate the liver’s ability to produce clotting factors.
- Serology: Blood tests for viral hepatitis markers (e.g., hepatitis B and C) are essential to identify infectious causes.
- Autoantibodies: Testing for autoantibodies can help diagnose autoimmune-related ALF.
- Toxicology Screen: Detecting drugs or toxins in the bloodstream is crucial, especially in cases of drug-induced liver injury.
- Imaging Studies
- Ultrasound: Abdominal ultrasound can assess liver size, look for structural abnormalities, and identify ascites.
- CT or MRI: These imaging techniques may be used to evaluate liver and surrounding structures, helping to identify any structural abnormalities.
- Liver Biopsy
While less common, a liver biopsy may be necessary in certain cases to assess the degree of liver damage and identify the underlying cause.
The results of these diagnostic tests guide healthcare providers in diagnosing the cause of ALF and determining the appropriate treatment approach.
Conventional Treatment for Acute Liver Failure
The treatment of ALF is multifaceted and varies depending on the underlying cause, severity of the condition, and the patient’s overall health. Common interventions include:
- Supportive Care
- Hepatic Encephalopathy Management: Medications like lactulose or rifaximin are used to manage hepatic encephalopathy.
- Nutritional Support: Intravenous (IV) nutrition is often necessary, as patients with ALF may have difficulty eating.
- Identifying and Managing the Underlying Cause
- Viral Hepatitis: For cases of ALF caused by viral hepatitis, antiviral medications may be used.
- Drug-Induced Liver Injury: Identifying and discontinuing the causative medication is crucial.
- Autoimmune Hepatitis: Steroid medications like prednisone are used to manage autoimmune hepatitis.
- Liver Transplantation
Liver transplantation is considered for severe cases of ALF, especially when other treatments fail or the condition is rapidly deteriorating.
- Monitoring and Surveillance
Regular monitoring of liver function, coagulation parameters, and clinical status is essential to assess the patient’s response to treatment and make timely decisions regarding transplantation.
Prevention of Acute Liver Failure
Preventing ALF depends on understanding and mitigating risk factors:
- Vaccination
- Hepatitis A and B vaccines can prevent some forms of viral hepatitis, a common cause of ALF.
- Medication Safety
- Patients and healthcare providers should exercise caution when prescribing or taking medications that have potential liver toxicity.
- Avoiding Excessive Alcohol Consumption
- Limit alcohol intake to prevent alcoholic liver disease, which can lead to ALF.
- Early Identification of Liver Conditions
- Identifying and managing chronic liver conditions, such as hepatitis and Wilson’s disease, can help prevent progression to ALF.
Herbal Medicines for Acute Liver Failure
Complementary and alternative therapies, including herbal remedies, are sometimes considered as adjunct treatments for ALF. However, the use of herbal medicines in ALF should be approached with caution and under the guidance of healthcare professionals. Some herbs and supplements that have been studied for their potential benefits in liver health include:
- Milk Thistle (Silymarin)
Milk thistle is one of the most widely used herbal remedies for liver conditions. It has antioxidant and anti-inflammatory properties and is believed to protect liver cells.
- Artichoke (Cynara scolymus)
Artichoke extract is thought to support liver function by enhancing bile production and improving digestion.
- Turmeric (Curcumin)
Curcumin, the active compound in turmeric, is known for its anti-inflammatory and antioxidant properties. It may benefit liver health.
- Dandelion (Taraxacum officinale)
Dandelion root is believed to have diuretic properties and may support liver health.
- Schisandra (Schisandra chinensis)
Schisandra is an adaptogenic herb that may protect the liver from various toxins.
It’s important to emphasize that while these herbal remedies have shown promise in some studies, their effectiveness can vary between individuals. Consult a healthcare provider before using herbal medicines, especially if you have existing medical conditions or are taking other medications.
Lifestyle Modification for Acute Liver Failure
Lifestyle modifications are essential for preventing ALF and supporting recovery for individuals with liver conditions:
- Alcohol Abstinence
- Completely abstain from alcohol if you have liver disease, as alcohol can exacerbate liver damage.
- Medication Safety
- Follow your healthcare provider’s guidance regarding the safe use of medications, especially if you have a pre-existing liver condition.
- Maintain a Healthy Diet
- A well-balanced diet that is low in processed foods and rich in fruits, vegetables, and whole grains can support overall liver health.
- Weight Management
- Maintain a healthy weight to reduce the risk of non-alcoholic fatty liver disease (NAFLD).
- Exercise
- Regular physical activity can help improve overall health and support liver function.
- Stay Hydrated
- Drinking enough water is crucial for overall health, including liver function.
Conclusion
Acute Liver Failure is a serious and often life-threatening condition that requires immediate medical attention and appropriate treatment. Understanding the causes, clinical presentation, and treatment options is essential for both healthcare professionals and patients.
Complementary therapies, including herbal remedies, may offer some benefits in supporting liver health, but their use should be approached with caution and under the guidance of healthcare providers.
In conclusion, living with or recovering from ALF is a challenging journey. It is essential to work closely with healthcare providers, adhere to prescribed treatments, and make necessary lifestyle modifications to optimize liver health and overall well-being. Early diagnosis and appropriate management are key to preventing complications and ensuring a better quality of life for those affected by this condition.