Unraveling Epilepsy: A Comprehensive Journey from Clinical Diagnosis to Holistic Management for Enhanced Quality of life
Introduction
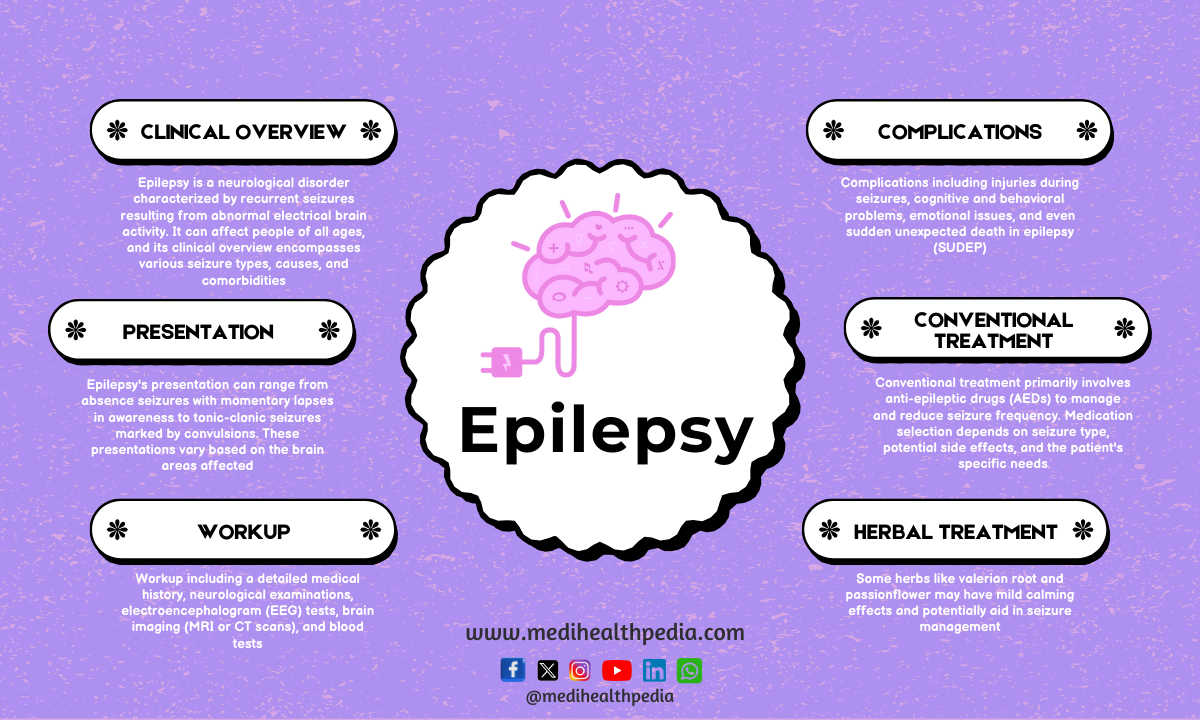
Epilepsy is a multifaceted neurological disorder that affects millions of individuals worldwide. Characterized by recurrent, unprovoked seizures resulting from abnormal brain activity, epilepsy’s intricacies encompass a wide range of seizure types, causes, and treatment approaches. In this comprehensive article, we will delve into the clinical overview of epilepsy, the diverse clinical presentations, essential diagnostic investigations, potential complications, established conventional treatments, preventive strategies, the role of herbal medicines in treatment, and the transformative impact of lifestyle modifications. By the end, we hope to provide a holistic understanding of epilepsy and empower individuals with the knowledge needed for a better quality of life.
Clinical Overview of Epilepsy
Understanding the clinical overview of epilepsy is foundational to comprehending this neurological condition:
- Definition: Epilepsy is a neurological disorder characterized by recurrent and unprovoked seizures.
- Prevalence: It affects people of all ages and is the fourth most common neurological disorder worldwide.
- Classification: Epilepsy is classified into different types based on seizure patterns and underlying causes.
- Triggers: Seizures may be provoked by a variety of factors, including sleep deprivation, stress, or certain medications.
Clinical Presentation of Epilepsy
Epilepsy’s clinical presentation is a complex interplay of seizure types, each with its own unique characteristics:
- Convulsive seizures: These involve muscle stiffness, jerking, and loss of consciousness, with grand mal seizures being a notable example.
- Non-convulsive seizures: These may lead to altered awareness or unusual behaviors, such as complex partial seizures.
- Absence seizures: Brief episodes of staring into space and altered awareness are hallmark features.
- Tonic seizures: Characterized by sudden muscle stiffness and potential falls.
- Atonic seizures: These lead to a sudden loss of muscle tone, potentially causing falls or accidents.
- Myoclonic seizures: Sudden, brief muscle jerks are a distinctive feature.
Basic Investigations for Epilepsy
Accurate diagnosis of epilepsy involves a combination of clinical assessments and tests:
- Electroencephalogram (EEG): This measures electrical activity in the brain and is instrumental in detecting abnormal patterns indicative of epilepsy.
- Imaging: Brain MRI or CT scans are used to identify structural abnormalities and rule out other neurological conditions.
- Blood tests: These help to exclude metabolic or infectious causes for seizures.
- Video monitoring: Continuous video recording during seizures provides crucial data on seizure type, origin, and progression.
- Neuropsychological tests: These assess cognitive function and memory, identifying potential cognitive impairments.
Complications of Epilepsy
Epilepsy can introduce various complications and challenges for individuals living with the condition:
- Physical injuries: Seizures can lead to falls and injuries, emphasizing the importance of a safe living environment.
- Emotional impact: Epilepsy may result in anxiety, depression, or social isolation, underscoring the need for robust emotional support systems.
- Cognitive issues: Epilepsy can affect memory and cognitive function, requiring cognitive rehabilitation for some individuals.
- Medication side effects: Antiepileptic drugs (AEDs) may have side effects, necessitating close monitoring and potential adjustments.
- Status epilepticus: This life-threatening condition is marked by prolonged seizures and requires immediate medical attention.
Conventional Treatment of Epilepsy
Management of epilepsy typically centers on the use of antiepileptic drugs (AEDs) and other medical interventions:
- Medications: AEDs are tailored to seizure type and frequency, with regular monitoring of drug levels to optimize therapy.
- Vagus Nerve Stimulation (VNS): A surgically implanted device that stimulates the vagus nerve to reduce seizures, particularly in individuals who do not respond to AEDs.
- Responsive Neurostimulation (RNS): An implant that detects and responds to abnormal brain activity, delivering targeted stimulation to interrupt seizure activity.
- Epilepsy surgery: A potential option for individuals who do not respond to medications or who have specific epilepsy syndromes localized in one area of the brain.
Prevention of Epilepsy
While epilepsy itself is not always preventable, addressing potential risk factors and triggers is essential:
- Head injury prevention: Use of helmets and seat belts in high-risk situations.
- Seizure triggers: Effective stress management, adherence to sleep schedules, and avoidance of medications or substances that may provoke seizures.
- Medication adherence: Taking prescribed AEDs consistently to maintain seizure control and prevent breakthrough seizures.
Herbal Medicines for Epilepsy Treatment
While herbal remedies are not a substitute for conventional treatment, some herbs have shown potential benefits in managing seizures:
- Cannabidiol (CBD): Derived from cannabis, CBD has gained attention for its potential antiepileptic properties, particularly in certain epilepsy syndromes.
- Valerian root (Valeriana officinalis): Known for its calming effects, it may help reduce seizure frequency in some individuals.
- Kava (Piper methysticum): A traditional Polynesian herb believed to have antiepileptic properties, although caution is advised due to potential liver toxicity.
Consultation with a healthcare provider is paramount before integrating herbal remedies into an epilepsy management plan, as they may interact with AEDs and necessitate careful dosing.
Lifestyle Modification for Epilepsy Management
Individuals with epilepsy can make meaningful lifestyle changes to support their well-being and seizure management:
- Medication adherence: Taking prescribed AEDs as directed and monitoring drug levels regularly.
- Stress management: Incorporating relaxation techniques, mindfulness practices, and regular exercise to reduce stress, a known seizure trigger for many.
- Sleep regulation: Maintaining a consistent sleep schedule and prioritizing restful sleep to minimize seizure occurrence.
- Dietary choices: Avoiding excessive alcohol and caffeine intake, as these substances can trigger seizures in some individuals.
Conclusion
Epilepsy is a multifaceted neurological disorder, impacting individuals in a myriad of ways. A comprehensive understanding of its clinical overview, clinical presentation, and diagnostic procedures is essential for developing effective management strategies. While conventional treatments, primarily antiepileptic drugs, remain the mainstay of therapy, exploring preventive measures, herbal remedies, and lifestyle modifications can offer valuable complementary support.